
Lea esta hoja informativa en español
Table of Contents
Pain is common in people living with HIV. It can occur at all stages of HIV disease and can affect many parts of the body. Usually pain occurs more often and becomes more severe as HIV disease progresses, especially if it is not being treated. But each individual person is different. While some people may experience a lot of pain, others have little or none. The good news is that, as HIV treatments have improved, fewer people living with HIV are experiencing pain.
What Causes Pain?
HIV-related pain may be:
- A symptom of HIV itself
- A symptom of other illnesses or infections
- A side effect of HIV drugs
Regardless of its cause, pain should be evaluated and treated to help you have a good quality of life.
Common Types of Pain
The first step in managing HIV-related pain is to identify the type, and if possible, the cause of pain. Some common types of pain – not necessarily HIV-related -- include the following:
- Peripheral Neuropathy – Pain due to nerve damage, mostly in the feet and hands. It may be described as numbness, tingling, or burning. Nerve damage can be caused by HIV itself, HIV drugs, or other medical conditions such as diabetes. The older HIV drugs that caused the most peripheral neuropathy – d4T (Zerit) and ddi (Videx) – are rarely used today.
- Abdominal Pain – There are many possible causes of abdominal pain (pain in the stomach area):
- A side effect of some HIV drugs (for example, cramps)
- Infections caused by bacteria or parasites
- Problems of the digestive tract (gut), such as irritable bowels
- Inflammation of the pancreas (pancreatitis) can be caused by some HIV drugs, high levels of fat in the blood, or drinking alcohol
- Bladder or urinary tract infections (especially in women)
- Menstrual cramps or conditions of the uterus (womb), cervix (opening to the womb), or ovaries
- Headache – Head pain can be mild to severe, and may be described as pressure, throbbing, or a dull ache. The most common causes of mild headaches include muscle tension, flu-like illness, and side effects of HIV drugs. Moderate or severe headaches can be caused by sinus pressure, tooth infections, brain infections, brain tumors, bleeding in the brain, migraines, or strokes.
- Joint, Muscle, and Bone Pain – This pain can also be mild to severe. It may be related to conditions such as arthritis, bone disease, injury, or just aging. It can also be a side effect of some HIV drugs and medications for other conditions, such as hepatitis or high cholesterol.
- Herpes Pain– Herpes is a family of viruses common in people living with HIV. Herpes viruses stay in the body for life, going into hiding and coming back later. The varicella-zoster herpes virus first causes chickenpox and later can cause shingles, a painful rash along nerve pathways. Herpes simplex virus types 1 and 2 cause painful blisters around the mouth ("cold sores") or genital area. Even after a herpes sore heals, the pain may continue.
- Other Types
- Painful skin rashes due to infections or side effects of HIV drugs or other drugs
- Chest pain caused by lung infections such as TB, bacterial pneumonia, or PCP pneumonia (Pneumocystis pneumonia)
- Mouth pain caused by ulcers ("canker sores") or fungal infections like thrush
- Fibromyalgia or related chronic pain conditions
- Pain due to cancer anywhere in the body
Assessing Pain
The goals of pain assessment are to:
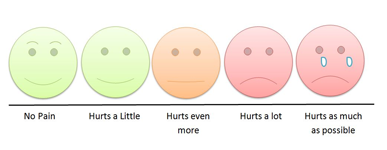
- Define the severity of the pain (how much it hurts): Your healthcare provider may ask you to assign a number to your pain, from one (very mild pain) to ten (the worst possible pain). Pictures can also describe pain. A smiling face represents little or no pain, while a crying face represents severe pain.
- Describe details of your pain: Your healthcare provider may ask you to describe how your pain feels, for example sharp, dull, throbbing, aching, or burning. Is it new (acute) or have you had it for a while (chronic)? Where is it located? Is it constant, or does it come and go? Does anything make it worse or better?
You may be having pain and do not want to complain about it. Or perhaps you do not want to talk about your pain because you are afraid to know what is causing it. However, pain is your body's way of telling you that something is wrong. Talking to your healthcare provider about how you feel is not complaining – it is the best thing you can do to find out what is wrong and get the right treatment.
Pain Management
Once the type and characteristics of pain are identified, you and your healthcare provider will decide how to manage or treat it. The following factors will play a role in choosing the right type of treatment for you:
- Cause, type, and severity of pain
- Whether it is short-term or long-term
- Whether you have ever been addicted to or dependent on prescription medications or street drugs (substance abuse)
If your pain is caused by a medication you are taking or by another illness, your healthcare provider may want to take care of that first. If you are still experiencing pain, there are many options for pain relief.
Non-Medicinal Therapies
Pain relief options without medications include:
- Massage
- Relaxation techniques, such as meditation
- Physical therapy
- Acupuncture or acupressure
- Heat and cold therapy
- Hypnosis
- Mental imagery or visualization
- Regular physical activity, including stretching and yoga
- Cognitive Behavioral Therapy
- Stress reduction
- Distraction
Many of these options – such as massage, acupuncture, meditation, and exercise — trigger the body to release endorphins. Endorphins are brain chemicals that act similar to drugs such as morphine and codeine. While these therapies may be enough to relieve pain by themselves, they are often used along with pain medications. For more information, see our fact sheet on Complementary Therapies.
Non-Opioid Medications
These are pain relief medicines that do not contain narcotics (opiates). They are available over the counter or by prescription. These medicines relieve mild to moderate pain related to inflammation or swelling. Some people with a history of substance use prefer these non-opioid pain medicines. They include:
- Tylenol (acetaminophen)
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen (e.g., Advil), naproxen (e.g., Midol) or meloxicam
- COX-2 inhibitor, a type of NSAID that is less likely to cause stomach problems, e.g., Celebrex (celecoxib)
- Steroids, which are natural or manufactured hormones that reduce inflammation, thereby reducing the severity of pain. Examples include prednisone and hydrocortisone.
- Lyrica, a medicine that is used to treat nerve and muscle pain.
Non-opioid pain medicines can cause side effects, including liver damage (Tylenol), easy bleeding (aspirin), stomach pain or damage (aspirin and other NSAIDs), heart problems (COX-2 inhibitors), and high blood sugar and bone weakening (steroids).
Opioids/Narcotics
Narcotics and related drugs known as opioids are the strongest pain relievers and are available by prescription. They are used to treat moderate to severe pain.
Opioids are grouped, or classified, by how fast and how long they work.
- Immediate release opioids – work quickly but pain relief lasts for a shorter time
- Sustained-release opioids – take longer to start working but pain relief lasts longer
Opioids are also classified by their strength.
- Moderate pain relievers (they are often mixed with non-opioid medicines to improve their action):
- Hydrocodone
- Vicodin (hydrocodone plus acetaminophen)
- Codeine
- Tylenol with codeine (acetaminophen plus codeine)
- Ultram (tramadol)
- Severe pain relievers:
- Percocet (acetaminophen and oxycodone)
- Morphine
- Duragesic (fentanyl)
- OxyContin (oxycodone)
- Dilaudid (hydromorphone)
- Methadone or Buprenorphine (reserved for treatment of pain that does not respond to other pain relievers)
Opioids can cause side effects, including drowsiness, nausea, and constipation. Overdoses can slow down breathing and cause death. Opiates can lead to dependence or addiction and may be a problem for people with a history of substance use. Opiates are not recommended for chronic pain and are generally only used for short-term pain relief of less than a week, usually after a major surgery.
A drug called naloxone can help prevent death from overdose. Guidelines from the World Health Organization recommend that countries expand naloxone access to people who are likely to witness an overdose in their community and are in a position to quickly help someone experiencing an overdose, such as friends, family members, partners, and social workers of people who use drugs. In the US, some first responders (emergency workers) carry naloxone, and in some areas, training on administering the drug, as well as naloxone kits, is available to laypersons.
Topical or Local Therapies
These are medications that are injected or applied to the skin around a painful area. Examples include the local anesthetic Xylocaine (lidocaine, comes in patches or creams), Voltaren (a topical NSAID), menthol, and capsaicin, which comes from chili peppers. Steroids can also be injected into painful joints by certain healthcare providers and provide pain relief.
Other Therapies
There are medicines prescribed for other purposes that also relieve pain.
- Anti-depressants – can also relieve nerve pain such as peripheral neuropathy. Some examples are Pamelor (nortriptyline), Elavil (amitriptyline), and Cymbalta (duloxetine).
- Anti-convulsants – used to treat seizures but can also help with peripheral neuropathy and herpes pain. Examples include Neurontin (gabapentin), Tegretol (carbamazepine), Topomax (topiramate), and Trileptal (oxcarbazepine).
Determine if the Pain Treatment Works
Once you start medication or other pain treatment, your healthcare provider will likely check your pain regularly to see if the treatment is working. Sometimes pain medications can stop working over time.
What to Do if You Have Pain
When you experience pain, it is important to know how to get safe relief.
- Do not ignore your pain – Pain is the body's way of telling you something is wrong. Ignoring pain often makes matters worse and can cause more damage in the long run.
- Assess your pain – When pain occurs ask yourself the following questions:
- How long have I had the pain?
- Did it happen suddenly or over time?
- Is the pain sharp or dull?
- What makes the pain worse?
- Does anything make it better?
- Is the pain limited to one place or does it spread out to other areas?
- Are there other symptoms (for example numbness, cough, or fever)?
- Tell your healthcare provider – Report pain to your provider without delay. Describing your pain will help find the cause and how best to treat it.
- Take your pain medicine as directed – Pain medications work best if they are taken at the first sign of pain. Waiting until the pain is very bad before taking pain medicine, or "toughing it out", is not helpful.
- Be responsible – Pain medications are very effective when taken as prescribed. Taking them incorrectly can be dangerous. Opioids are addictive, meaning you can develop physical and emotional dependence on a drug. High doses can cause breathing problems. In the worst cases, incorrect use of opioids can be fatal (can cause death). Opioids are also controlled substances, which means that their distribution, possession, and use are controlled by the government and your healthcare provider must write the prescription. It is illegal in the US to sell or share your opioid pain medications with others.
- Tell your healthcare provider if you still have pain while taking medication for it. You may be taking a medication that will not work for you, or your body may have gotten used to the medication (has built a tolerance to the drug). You may need to change doses or switch to a different type of treatment.
Pain is common among people living with HIV. However, it can be managed using a variety of methods. Talk to your healthcare provider if you are having pain. He or she can work with you to find the cause, manage the pain, and improve your quality of life.

