Lea esta hoja informativa en español
Table of Contents
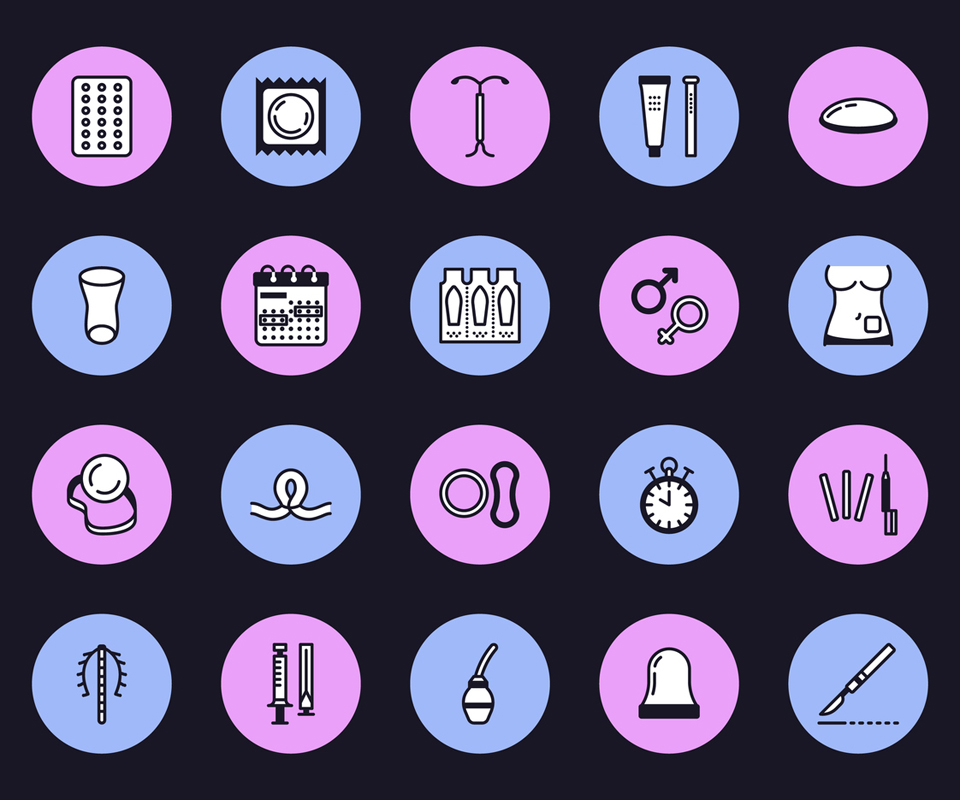
- Women Living with HIV and Contraception
- Methods That Prevent Pregnancy and Protect Against HIV
- Hormone-Based Methods That Prevent Pregnancy but Do Not Protect Against HIV
- Non-Hormonal Methods That Prevent Pregnancy but Do Not Protect Against HIV
- Benefits and Drawbacks to Some Contraceptive Methods
- Contraception Is Different from Abortion
- How to Choose a Contraceptive Method
- The Future: Multipurpose Prevention Technologies
Women Living with HIV and Contraception
Women living with HIV who do not use condoms and do not want to get pregnant (or make someone pregnant) have several other choices.
All people who are physically able to become pregnant – and are sexually active with people who are physically able to get someone pregnant – need to make decisions about whether to take steps to avoid pregnancy (contraception; also known as "birth control"). This includes cisgender women, transgender (trans) men, and other people who have uteruses who:
- have sex with cisgender men, trans women, or other people who have penises and
- have not yet completed menopause (12 months without any periods) or
- have not had surgery that prevents pregnancy
It is also important for each person to decide which method of contraception is best for them.
If you are a woman living with HIV, it is also important to consider the possibility of passing HIV to a partner. Recent research has shown that you cannot transmit the virus to a sexual partner who is not living with HIV, if you are taking HIV drugs and your viral load is undetectable (not enough HIV in your blood for a standard test to measure). For more information on this, see our fact sheet Undetectable Equals Untransmittable: Building Hope and Ending HIV Stigma.
When both partners are living with HIV, you do not need to worry about one person acquiring HIV from the other. However, one partner could transmit a strain of HIV that is resistant to the other partner's prescribed HIV drugs (also called superinfection). Also, other sexually transmitted infections or diseases (STIs or STDs) could be passed from one partner to the other. The only existing forms of contraception that will provide protection against HIV and most other STIs are abstinence (not having sex) or using condoms or other barriers while having sex.
Not all women living with HIV will want to, or be able to, have their partners use condoms, whether their partners are living with HIV or not. If you would like to use condoms but are having trouble talking to your partner about using them, see our fact sheet on Talking with Your Partner about Condoms.
Women living with HIV who do not use condoms and do not want to get pregnant (or make someone pregnant) have several other choices. These other methods of contraception offer protection against pregnancy, but do not protect against HIV or other STIs. Some healthcare providers suggest "dual (double) protection" – condoms to prevent STI/HIV transmission, and another method to prevent pregnancy.
Methods That Prevent Pregnancy and Protect Against HIV
Condoms
Condoms (rubbers) are thin latex or plastic barriers. The "male" condom (also called an external condom, because it is worn on the outside of the body) is worn on the penis. The "female" condom (also called an internal condom, because it is worn inside the body) is put in the vagina or anus (butt).
Benefits:
- Condoms are the most effective ways to prevent many STIs (including HIV)
- If used correctly and every time, external condoms are up to 98 percent effective at preventing pregnancy; if not always used correctly, external condoms are only 85 percent effective
- If used correctly and every time, internal condoms are up to 95 percent effective at preventing pregnancy; if not always used correctly, internal condoms are only 79 percent effective
- The internal condom is the only contraceptive method that is controlled by the receptive partner and also provides protection from STIs
- Internal condoms can be inserted several hours to immediately before sex
- External condoms are inexpensive compared to other forms of contraception
- Condoms do not require a prescription
Drawbacks:
- An external condom requires the partner with a penis to cooperate
- External condoms may break if worn incorrectly
- Latex condoms may break if used with oil-based lubricants such as baby oil or Vaseline. Do not use oil-based lubricants with condoms made of latex.
- External condoms must be put on during sex while a partner's penis is erect
- Internal condoms can be more expensive than external condoms and are not available everywhere
The external condom is available in lubricated and unlubricated (dry) forms. Unlubricated condoms are often the condoms of choice for oral sex. For vaginal sex, you can use either a lubricated or unlubricated condom. For anal sex, experts suggest using lubricated condoms. You can choose to add lubricant (lube) any time you use a condom. Remember, however, to use only water-based lubes (like Astroglide and KY Jelly) with latex condoms. Oil-based lubricants, such as mineral oil, cold cream, Vaseline (petroleum jelly), and vegetable oils, will damage latex. The condom may no longer prevent infections or pregnancy.
Condoms lubricated with the spermicide Nonoxynol-9 (N-9) are no longer recommended. They have a shorter shelf life, do not lower the risk of pregnancy more than other lubricated condoms, and may increase vulnerability to HIV by causing irritation of the vagina or rectum (butt).
Hormone-Based Methods That Prevent Pregnancy but Do Not Protect Against HIV
Hormone-based contraceptives are available in progesterone-only or combined estrogen and progesterone versions. Hormone methods are available in many different forms, including pills, shots (injections), implants, vaginal rings, patches, and most types of intrauterine devices (IUDs). Depending on which you choose, you will need to use hormone-based methods daily, weekly, monthly, or every few months or years. You need a prescription for hormonal methods. For some methods, a healthcare provider must regularly give you a shot or insert an implant or IUD.
Some HIV drugs decrease the levels of hormone-based contraception and could increase the chances of an unwanted pregnancy.
A study of more than 5,000 African women living with HIV showed that, regardless of whether or not women were taking HIV drugs, hormone-based methods were effective in preventing pregnancy. Specifically, implants appeared to be the most effective (greater than 90 percent), with injectable methods coming in a close second (just over 80 percent), and oral contraceptives finishing third (approximately 60 percent). IUDs and implants are by far the most effective forms of contraception, partly because their protection lasts for a long time.
Interactions with HIV Treatment
There are several ways in which some hormone-based contraceptive methods can interact with HIV drugs. Some HIV drugs decrease the levels of hormone-based contraception and could increase the chances of an unwanted pregnancy. However, there are no studies that have shown that these drug interactions actually do increase the chances of pregnancy.
Some HIV drugs increase the levels of hormone-based contraceptive methods. It is not clear what effect this may have. It is important to talk with your healthcare provider to see whether or how your HIV drugs interact with your preferred method of pregnancy prevention. Your provider should know how to adjust the doses of your HIV drugs and/or hormone-based contraceptive methods. The hormone-based methods least likely to be affected by your HIV treatment are DMPA (DEPO), Nexplanon (implant), and IUDs.
After reviewing the scientific data, the World Health Organization (WHO) recommended in June 2014 that women living with HIV and women highly vulnerable to acquiring HIV can continue to safely use hormonal contraceptives. This is so because there are no studies showing that interactions between HIV treatment and hormonal contraceptive methods definitely increase the chance of pregnancy.
The WHO did recommend that special consideration be given to women taking Sustiva (efavirenz) or Viramune (nevirapine). In 2014, researchers in one study found the NNRTI Sustiva reduced the effectiveness of a commonly used progesterone contraceptive implant among women living with HIV in Uganda. Sustiva is used widely in resource-limited areas. Therefore, it is important that women and their healthcare providers be aware of Sustiva's effect on progesterone-containing contraceptive implants.
In the US, some combinations of hormonal contraceptives, such as pills containing ethinyl estradiol, and certain antiretrovirals, such as Prezista (darunavir), are not recommended. Make sure all your healthcare providers know about all drugs you are taking.
Effects on Acquiring HIV
In the past few years, there has been some debate about the effect of hormonal contraceptives, such as the pill or injectable Depo-Provera (DMPA), on HIV transmission. It appears fairly clear from available data that oral hormonal contraceptives ("birth control pills") do not increase women's chances of acquiring HIV. However, it remains unclear whether DMPA increases women's chances of acquiring HIV. Therefore, if you are using DMPA to prevent pregnancy, experts recommend that you also use condoms to protect against acquiring HIV.
Remember, treatment for the partner living with HIV so they have an undetectable viral load (treatment as prevention), or, if you are HIV-negative, pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP), are effective HIV prevention strategies.
Long-Acting Reversible Contraceptives (LARCs)
According to the American College of Obstetricians and Gynecologists (ACOG), IUDs and implants are by far the most effective forms of contraception – 20 times more effective than contraceptive patches, rings, or pills. During the first year of using an IUD or an implant, typically fewer than one in 100 women will become pregnant.
IUDs (Intrauterine Devices)
An IUD is a small, T-shaped device put into the uterus (womb) by a healthcare provider. Several types of IUDs are currently available. Mirena, Skyla, and Liletta are IUDs that contain levonorgestrel, a hormone similar to that found in contraceptive pills. The hormone is released over time and prevents pregnancy. Mirena lasts for five years, while Skyla and Liletta each last for three years. ParaGard is a non-hormonal IUD that contains copper and lasts for ten years. Any of these IUDs can be removed at any time if you want to switch contraceptive methods or become pregnant.
Implants
Contraceptive implants are thin, flexible plastic rods that are inserted under the skin of the upper arm. An implant is about the size of a matchstick and contains a form of the female sex hormone progesterone. It can last up to three years. The most common implant is Nexplanon.
Shots (Injections)
Contraceptive shots are injections of a form of the female sex hormone progesterone. The shots last for up to three months. The most common shot is Depo-Provera, or DMPA (depot medroxyprogesterone acetate). Because researchers are unclear if using DMPA increases women's chances of acquiring HIV, it is especially important to use additional methods to prevent HIV acquisition. These include condoms, treatment of the partner living with HIV (treatment as prevention), and pre-exposure prophylaxis (PrEP) if you are not living with HIV.
Patches and Rings
Contraceptive patches are thin, flexible plastic squares that stick to the skin and release forms of the female sex hormones progesterone and estrogen. They are good for one week each and are applied for three weeks in a row followed by one week off. The patches are known by the name Ortho Evra or Evra.
Contraceptive rings are small, flexible rings that women insert deep into their vagina. One ring is good for three weeks, after which there is a week without a ring. Commonly known as NuvaRing, it contains forms of the female sex hormones estrogen and progesterone.
Oral Contraceptive Pills ("Birth Control Pills")
Contraceptive pills (or "the pill") are a type of medication women can take by mouth to prevent pregnancy. They contain either progesterone only, or a combination of estrogen and progesterone. Combination pills come in 21-day or 28-day packs, and each type of pack contains 21 pills with active hormones (28-day packs also come with 7 days of placebo – inactive – pills). With combination pills, you take 21 days in a row of a pill containing hormones, then take 7 days off. Progesterone-only pills come in packs of 28 active pills that you take every day (no days off).
Emergency Contraception
There are two methods that help prevent pregnancy after unprotected sex or condom failure: emergency "morning after" pills and emergency IUD insertion.
While these methods can be effective in reducing the risk of pregnancy if started within a few days after sex, it is important to note that they offer no protection against STIs (including HIV). An IUD can be up to 99 percent effective in preventing pregnancy if it is inserted within five to seven days after sex. It works by stopping the implantation of a fertilized egg in the uterus (womb).
Having methods that combine prevention of pregnancy and STIs (including, but not limited to HIV) would be more convenient and likely lead to more consistent, and therefore more effective, use.
There are several types of "morning after" pills. The first is a pill containing a synthetic (manufactured) version of the female sex hormone progesterone. This pill has several names, including Plan B One-Step in the US, Levonelle in the UK, Escapelle in South Africa, and Unwanted 72 or i-Pill in India. These pills should be taken as soon as possible, since their effectiveness depends on how soon you take them. If taken within 72 hours of sex, they can reduce the chance of pregnancy by close to 90 percent. Researchers are unsure if taking HIV drugs reduces the effectiveness of "morning after" pills; it is best to continue taking your HIV drugs as usual if you use "morning after" pills.
The second type of "morning after" pill is called Ella (in the US, or EllaOne in the European Union). It contains ulipristal, which is another form of progesterone. Ella needs to be taken within five days of sex.
Morning after pills do not cause abortion. They only work if you are not already pregnant.
Non-Hormonal Methods That Prevent Pregnancy but Do Not Protect Against HIV
Diaphragms and Cervical Caps
The diaphragm and cervical cap fit over the cervix, the passageway between the vagina and uterus (womb). Both the diaphragm and cap need to be fitted by a healthcare provider and used with a spermicidal cream, jelly, or foam (see note below regarding the spermicide N-9).
Spermicides
Spermicides are available in a variety of forms such as film, foam, jelly, cream, sponge, and suppository.
Warning: The spermicide Nonoxynol-9 (N-9) can actually increase the risk of acquiring HIV by irritating the skin in the vagina and rectum. Condoms with nonoxynol-9 are no longer recommended for this reason. If you are HIV-negative, you may want to explore other options for preventing pregnancy.
Permanent Contraception (Sterilization)
Sterilization is a surgical procedure that can be performed on a person with a uterus (tubal ligation) or a person with a penis (vasectomy). It is almost 100 percent effective against pregnancy; however, it is not effective against STIs (including HIV). It can generally not be reversed, if you change your mind about becoming pregnant.
"Natural" Contraception
This includes abstinence, withdrawal, and fertility awareness-based methods, including the "Rhythm Method." The effectiveness of natural contraceptive options at preventing pregnancy ranges from 100 percent (abstinence) to 73 percent (withdrawal method). Except for abstinence, natural methods are not effective for preventing STIs (including HIV).
Benefits and Drawbacks to Some Contraceptive Methods
| Contraception type | Benefits | Drawbacks | Notes |
|---|---|---|---|
| Intrauterine devices (IUD) |
|
|
One specific form of IUD that does not involve hormones:
|
| Implants |
|
|
Less effective if person also takes Sustiva to treat HIV |
| Injections (shots) |
|
|
Least interaction with HIV drugs |
| Patches & rings |
|
|
If device contains estrogen, it should not be used by people with certain medical conditions |
| Oral contraceptives ("birth control pills") |
|
|
If pill contains estrogen, it should not be used by people with certain medical conditions |
| Diaphragms & cervical caps |
|
|
Contraception Is Different from Abortion
Stigma, confusion, and misinformation regarding sexual health and pregnancy are rampant online and elsewhere. For that reason, it is worth noting here that hormone-based contraception, including emergency contraception, is not the same as abortion. Abortion means the termination (ending) of a pregnancy. Contraception is the steps taken to keep a pregnancy from happening in the first place. The medications used for contraception are different from those used in medication abortion.
Abortion and contraception are both normal aspects of healthcare, though these practices are heavily restricted in many parts of the world. Please see our fact sheets Abortion and HIV and Abortion Laws and HIV in the US for more information on these topics.
How to Choose a Contraceptive Method
For women living with HIV, drug interactions and the need to reduce the chance of HIV transmission can complicate choosing a method to prevent pregnancy. Work closely with your healthcare provider or a family planning counselor to decide on the contraceptive method that is best for you.
It is important to get accurate and up-to-date information on any form of contraception you choose. You may want to ask the following questions about different methods:
- Does it provide protection from sexually transmitted infections (STIs) including HIV?
(Except for condoms, none of the current contraceptive options protect against STIs.) - Does it interact with my HIV drugs or other drugs I am taking?
- How well will it fit into my lifestyle?
- How convenient will it be?
- How effective is it?
- How safe is it?
- Will I like it?
- Will my partner like it?
- How affordable is it?
- How will it affect my chances of getting pregnant in the future if I choose to?
The Future: Multipurpose Prevention Technologies
Multipurpose prevention technologies (MPTs) provide ways of preventing more than one thing with one device. For example, MPTs may prevent pregnancy and HIV, or they may prevent HIV and several other STIs. Having methods that combine prevention of pregnancy and STIs (including, but not limited to HIV) would be more convenient and likely lead to more consistent, and therefore more effective, use. To learn more about MPTs and other HIV prevention methods that are being developed, see our fact sheet on Microbicides.
Researchers are studying several methods for combining prevention technologies, including a vaginal ring that contains both a hormonal contraceptive (to prevent pregnancy) and an HIV drug (to prevent HIV; this would be a form of pre-exposure prophylaxis, or PrEP). It can be inserted well before sex, stay there for up to three months, and is not usually felt by either partner. A vaginal ring just for HIV prevention has already been approved in South Africa and elsewhere, but not in the US.

