
Lea esta hoja informativa en español
Table of Contents
- How Often Should You Go?
- What to Expect in the Office
- A Checklist and Questions to Get Ready for Your GYN Visit
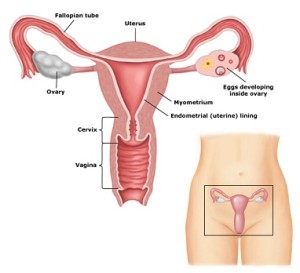
For people living with HIV, there are many aspects to staying healthy. You are off to a good start if you take your medications on schedule, eat well, and get regular physical activity. Part of taking care of your whole body is caring for your genital and reproductive health (whether or not you are able to or plan to be pregnant or get someone else pregnant). For anyone with a vagina, cervix, uterus, and/or ovaries, this means getting gynecologic care as part of routine health checkups from a health care provider. Gynecologic (GYN) care means screening for and treating health issues affecting the sexual and reproductive organs.
For people of all gender identities, preventive care and health screenings should be based on their sexual and reproductive organs. This fact sheet will focus on GYN care for people with a vagina, cervix, uterus, and/or ovaries. For women of trans experience, it may be a good idea to consult with your HIV care provider about inclusive, respectful, and knowledgeable care for your sexual and reproductive health.
How Often Should You Go?
It is very important for people living with HIV who have a cervix to have routine GYN visits and tests for cervical cancer. The US Centers for Disease Control and Prevention (CDC) recommends:
Women Ages 21 to 29 Years Old
- A complete gynecological examination, including a cervical screening test (e.g., Pap test) and a pelvic exam, when they are first diagnosed with HIV, and then another test 12 months later
- If the results of three tests in a row (consecutive tests) are normal, they should have another Pap test in three years, although they will generally still have a pelvic and breast exam every year
- Co-testing with Pap test and HPV test is not recommended for this age group
- If abnormal cells are found on the Pap test, a repeat test in six to 12 months is recommended if the person is HPV-negative or has not been tested for HPV. Your health care provider will tell you if further testing, such as a procedure called colposcopy, may be necessary.
Women 30 Years of Age and Older
- A complete gynecological examination, including a cervical screening test (e.g., Pap test only, or co-testing with Pap test and HPV test) and a pelvic exam, when they are first diagnosed with HIV, and then another test 12 months later
- If the results of three tests in a row are normal, they should have another Pap test in three years although they will generally still have a pelvic and breast exam every year
- If the Pap test is normal but they test positive for HPV, they should take both tests again in a year
- If abnormal cells are found in the follow-up Pap test, or they test positive for HPV, they should have a colposcopy to look at the cervix
Pregnant people living with HIV should have a cervical cancer screening test when they first seek prenatal care.
People who were born with HIV (acquired HIV at birth) are more likely to have high-risk types of HPV; therefore, they should have cervical cancer screenings before they are 21 years old if they are sexually active.
You should be tested for gonorrhea and chlamydia at your first gynecological visit. It is important to repeat these tests if you have a new partner, or if you have sex without condoms or other barriers. For more information about care and prevention of GYN issues, please see our fact sheet Common Gynecologic Concerns for People Living with HIV.
What to Expect in the Office
Usually, your health care provider will begin by asking you about your sexual history. You will be asked about:
- Your current sex life
- The number and genders of sexual partners in your past
- The type of sexual activities you engage in (e.g., oral, anal, vaginal sex)
- If you have any history of sexually transmitted infections or diseases (STIs or STDs)
- Whether you have ever been pregnant or had an abortion
- What kind of birth control you use, if any
- How you protect yourself and your partner(s) from STIs
- How you protect yourself (and possibly your partner or partners) from a different strain of HIV
These discussions can feel uncomfortable for both the provider and the patient. Even if it is difficult for you, do the best you can to provide honest responses. Your provider needs complete information to take good care of you.
Many people find the pelvic and bimanual exam slightly uncomfortable and embarrassing.
After the conversation, the provider will check different parts of your body. Not all providers perform all the exams listed below in the same order. The provider often asks a member of their staff (usually a medical assistant or nurse) to join them in your room for the physical exams. This is for everyone's protection and to make sure the exams are performed in a professional manner. It is also OK to request a same-gender provider, or to reschedule the physical exam for a different day if you are unable to see a provider of the gender you request.
Breast Exam
For the breast exam, the provider will ask you to lie back and raise one arm over your head as they feel with their hands for any lumps or masses in the breast on the side with your raised arm. The provider will then repeat this on the other side of your body, asking that you raise your other arm and feeling your other breast.
When you reach a certain age – usually between 40 and 50, depending on the country where you live – breast cancer screening with a mammogram is recommended. A referral for a mammogram often comes from a GYN provider.
Pelvic Exam
The provider will use a small brush, spatula, or swab to collect some cells from your cervix for the cervical cancer screening test.
For the pelvic exam, the provider will ask you to lie down and scoot your bottom to the end of the exam table. Then you will be asked to open your legs, bend your knees, and place your feet in the metal stirrups. Often, at this point, the provider will use their gloved fingers to examine the outside of your genitalia for any bumps, sores, or other problems. Next, your provider will insert an instrument called a speculum into your vagina. This instrument opens the walls of the vagina so that the provider can see your cervix (the opening to the uterus, or womb).
Then the provider will use a small brush, spatula, or swab to collect some cells from your cervix for the cervical cancer screening test. The cells will be sent to a laboratory, where they will be examined under a microscope to see if there are any abnormal cells (dysplasia). This is called a Pap test. Additional tests will be done if abnormal cells are found. While the speculum is still inserted, the provider may also collect fluid to check for infections.
The provider will use a small brush, spatula, or swab to collect some cells from your cervix for the cervical cancer screening test.
Because Pap tests require laboratories and people skilled in reading them, resource-limited countries offer different tests to check for dysplasia and cervical cancer. One method is called visual inspection with acetic acid, or VIA. When using VIA, health care providers swab acetic acid (vinegar) on the cervix and look directly at it to see if any areas need treatment. Other countries use HPV tests, which test samples taken from your cervix to see whether they contain specific strains of HPV's DNA (its genetic material) that can cause cancer.
Bimanual Exam
No speculum is used for the bimanual exam. In this exam, the provider places two gloved fingers inside your vagina and places the other hand on your belly. They feel your ovaries and uterus between their hands and check for any pain. The provider may also perform a rectal exam. During the rectal exam, the provider gently puts a lubricated, gloved finger into your rectum ("butt") to feel for any unusual bumps or sores. The provider may also collect a small amount of stool ("poop") to check for blood.
Many people find the pelvic and bimanual exam slightly uncomfortable and embarrassing. One reassuring thought is that the speculum is used for only two or three minutes, and the whole thing is usually over in less than five. And the more often you go, the easier it gets.
Anal Pap Smear
It is possible for people living with HIV of any gender to have abnormal cells (dysplasia) in their anus (butt-hole), which can lead to anal cancer. A rectal examination (checking your butt) with an anal Pap smear is the best way to find anal dysplasia. There are currently no official recommendations for anal Pap smear screenings among women living with HIV. Some providers perform this exam because of the higher risk for anal cancer among people living with HIV.
Similar to a cervical Pap smear, the provider inserts a small swab into the anus to collect cells. Some providers or clinics may allow you to collect a sample yourself by inserting a small swab into your own anus, about 2-3 inches deep, rotating the swab a few times and placing it in the specimen container. The cells are then sent to a laboratory, where they are examined under a microscope to see if there are any abnormal cells.
Similar to a cervical Pap smear, the provider inserts a small swab into the anus to collect cells.
It is important to remember that at any point during the breast, pelvic, bimanual, or anal exams, you can ask your provider to tell you what they are doing as it is happening. Some people find this helps them relax better throughout the exam. If you feel uncomfortable or uneasy at any part of the examination, you may ask your provider to stop or take a break. On some occasions, these particular examinations may bring up past sexual trauma or abuse. It is OK to acknowledge them and discuss your feelings with your provider.
A Checklist and Questions to Get Ready for Your GYN Visit
There are many things you can do to make your appointment with your GYN provider a smoother, easier, and more helpful visit.
Preparing your body
To get the best results from the physical exam part of your visit, it is important to do the following:
- Make sure you will not have your period during your visit; it is best to schedule your exam for one to two weeks after your period
- Do not douche or use other vaginal preparations for two to three days before your exam
- Do not have vaginal sex or sexual intercourse for 24 hours before your exam
- Wash your vaginal and rectal areas (your bottom) with water and soap or body wash before your exam
Preparing for your provider's questions
Your GYN care provider will ask you several questions about your sexual and medical history. These questions are not meant to invade your privacy or to criticize, but to gather important information to make good decisions about your health. It may be helpful to think about your answers before your appointment. Be prepared to answer the following questions:
- When did your last period begin?
- How long do your periods last?
- How often do they occur or how many days between periods?
- When did you have your last GYN exam (if you are seeing a new GYN provider)?
- Have you ever had any abnormal cervical screening (Pap) test results in the past? If you have, your provider will likely ask you when you had those abnormal test results, what those results were, and what treatments you received. You may find it easiest to bring copies of the reports. If you do not have copies of the reports, bring your previous GYN provider's contact information so that your new provider can get your past medical records from your previous provider. You will likely be asked to sign a medical release form that gives your new provider permission to ask your previous provider for your medical records.
- Have you noticed any changes in your menstrual cycle or periods (how much, how often, or how long)?
- Have you noticed any vaginal discharge? Vaginal odor? New lesions or sores?
- Have you had any lower belly or pelvic pain?
- Have you noticed any blood after sex or between periods?
- What other drugs and medications are you taking (including HIV drugs or gender-affirming hormone therapy)? For each drug, be sure to write down the name, dose, amount you take (number of pills or drops, amount of liquid), and when you take it. If you are not sure about your list or you are running late, put all your medications in a bag and bring them to your appointment so your provider can see exactly what you are taking. Make sure you also tell your provider about any other treatments or remedies you are taking – over-the-counter medications, herbal supplements, vitamins, teas, etc.
Preparing your questions
Whether or not you feel comfortable going to your GYN appointment, it is important that you write down a list of questions you want to ask your health care provider. Many people find it difficult to remember to ask their questions because so much goes on during the visit: the exam room, the change of clothes, the physical exam itself, and all the questions the provider asks! This is your opportunity to raise concerns and ask questions about the health of your body, so be ready with your list.
Things you may wish to talk about with your GYN provider:
- Getting vaccinated against hepatitis A, hepatitis B, or HPV
- Questions about birth control and contraceptive use
- How to improve the safety and satisfaction of your sex life
- Menstrual problems (how much, how often, how long)
- Urinary incontinence (leaking) or frequency (feeling that you need to pee often)
- How having been abused or assaulted (sexually or otherwise) in the past might affect your health now. While it may be a very uncomfortable thing to talk about, mentioning past trauma may help your provider better understand your symptoms and history and make a more accurate diagnosis.
- Things you can do to have good GYN and overall health
- How you will communicate with your provider after your visit, including if and how your provider will let you know the results of your exam
- Asking the provider to send you a copy of your results
If you have just had your GYN exam, congratulations! Regular GYN exams and cervical cancer screenings are very important to your health. Many GYN conditions do not have obvious symptoms and can get worse without your realizing it. Finding and treating GYN conditions in the early stages can prevent them from becoming more serious conditions later.
If your health care provider is not skilled in GYN care, or you would rather see a specialist, ask for a referral to a GYN care provider, preferably someone who is experienced in treating people living with HIV. If you receive GYN care from someone who is not your HIV provider, be sure that your HIV provider knows the results from your cervical screening tests, other GYN tests, and any treatments you might be taking for GYN conditions.

